The arthrosis of the knee joint is a chronic (longaster) degenerative disease that causes the destruction of the cartilage in the joints. Symptoms include pain, numbness and swelling.Hearing options for reducing pain and disability include changes in lifestyle (diet, physical exercise), physical and professional methods of treatment, medications and operations.
Symptoms include pain, numbness and swelling.Hearing options for reducing pain and disability include changes in lifestyle (diet, physical exercise), physical and professional methods of treatment, medications and operations.
Knee joint osteoarthrosis
The osteoarthrosis of the knee joint is common disease, followed by chronic, exhausting pain.Recent clinical data have shown that central sensitivity encourages deforming osteoarthritis of the knee joint.Improved understanding of how the knee joint arthrosis affects the central processing of pain is crucial to identify new analgesic goals / new therapeutic strategies.
Inhibitive cannabinoid receptors joject the function of peripheral immune cells and modulate the central neuro-immunometers in the models of neurodegenia.The system's introduction of agonist receptor has weakened pain behavior within the OA, and changes in the circulation of pro and anti-inflammatory cytokine is manifested in this model.
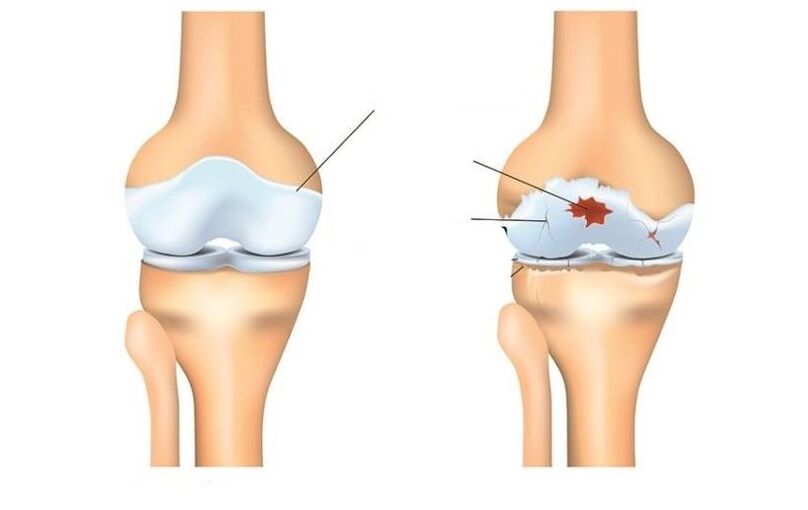
Deformation of arthrosis
Deforming Arthrosis The knee joint is inflammation and wear cartilage on the bones that make up the knee joint (osteo = bone, arthro = wrist, itis = inflammation).The diagnosis of osteoarthritis of the knee joint is based on two main results: Radiographic data changes in bone health (using medical images, such as X-rays and magnetic resonant image) and human symptoms.About 14 million people have a symptomatic arthrosis of the knee.Although more common in older people, two million of 14 million people with symptomatic oa knees were under 45 years, and during diagnosis, and more than half were under 65 years.
Osteoarthritis (oa knees) is a disease of processing caused by inflammation and degeneration of the knee joint, which is eventually worsening.
This affects the entire connection, including bones, cartilage, ligaments and muscles.His advancement affects age, body mass index (BMI), bone structure, geneticist, muscular strength and level of activity.The OA knee can also be developed as a medium state after knee injury.Depending on the disease phase and the presence of injuries or conditions associated with it, the OA knee can be controlled using physical therapy.Heavy or expanded cases may require surgical intervention.
Symptoms
People who develop the knee OA can have a wide range of symptoms and limitations based on the disease progress.The pain occurs when the cartilage covers the bones of the bone bone of the knee wrist.Areas in which cartilage is spent or damaged, exposes the bones below.The effect of the bone allows you to increase the stress and compression cartilage, and sometimes bones contact when you move, which can cause pain.Since the knee is common, the level of activity, the level of activity, as well as the type and duration of actions, usually have a direct effect on symptoms.Symptoms can worsen with weight, for example, when walking with a heavy object.
The symptoms of knee joints may include:
- During the operation during surgery or after surgery, especially when walking, climbing, lowering stairs or moving from a seated position.
- Pain or numbness after sitting with a bent or flat knee for a long time.The pain is the most common sense of osteoarthritis.As the disease progresses and inflammation progresses, pain can become constant.
- A feeling of jump, crack or grind when you move your knee.
- Swelling after action.
- The rigidity of the affected joint was often seen primarily in the morning and after rest.
- Edem, which is sometimes warm to the touch, can be noticed in the compound with arthritis.
- Deformation can occur with osteoarthritis due to the growth of bones and the loss of cartilage.The growth of bones in the end joints of the fingers are called Hyberden's knots.Rashar nodes are bone growth in the middle joints of the fingers.Degeneration of the cartilage of the knee joint can lead to the outer curvature of the knee (onions).
- Sound shooting or grate sensation may be noticed when arthritis moves.This is caused by erasing bones from bones or rough cartilage.
Usually these symptoms do not appear suddenly and all at once but gradually develop over time.Sometimes people don't admit to having osteoarthritis, because they can't recall a certain time or injury caused by their symptoms.If the pain in the knee worsened a few months, which does not respond to rest or change the activity, it is better to seek the advice of the medical worker.
Diagnostics
Osteoarthritis can often be diagnosed with characteristic pain symptoms, reduced movement and / or deformation.Osteoarthritis can be confirmed by X-ray or MRI scan.General data include narrowing space between bones, loss of cartilage and bones or bone growth.Blood tests can be used to exclude other possible conditions, but cannot diagnose osteoarthritis.

The OA knee is diagnosed with 2 primary process.The first is based on the symptoms and clinical examination report.The physiotherapist will ask questions about medical history and activities.The therapist will conduct a physical examination for measuring the movement of the knee (range of movement), strength, mobility and flexibility.They can also request various movements to see, increase or reduce pain.
Another tool used to diagnose your knee joint is diagnostic visualization.The physiotherapist can send a doctor who will prescribe X -Rays knees in various positions to check bone damage and the cartridge knee joint.
If more serious joint damage, you can order MRI to study the overall status of articular and surrounding fabrics more carefully.
Blood tests can also be ordered to release other conditions that can cause symptoms similar to osteoarthritis knee joints.
Treatment
Depending on the severity of the arthritis and the era of the patient, they will be selected how to treat the armrose of the knee joints.Treatment may consist of operational or inoperative methods or their combinations.
The first line of treatment of the wrist of the knee wrist includes the change of activity, anti -infalmator drugs and weight loss.Complete the action that improves pain can accept this state to some people.Anti-inflammatory drugs, such as ibuprofen and newer inhibitors COX-2, help mitigate inflammation that can contribute pain.
Physical therapy for strengthening muscle around the knee can help absorb part of the shock given to the community.This is especially true for arthritis with a knee cup (patello-femmeral).Special types of bras designed to transmit cargo on the part of the knee joint, which is less than arthritis, can also be alleged.Drug injections inside the knee joint can also be temporarily helped.
In addition, walking in a cane in the opposite side, because painful knee can help distribute part of the load, reducing pain.Finally, weight loss helps reduce the force passing through the knee joint.The combination of these inposite measures can help mitigate pain and disability caused by the arthritis of the knee joint.
If not inoperative methods do not allow you to stand tolerant, the operation can be the best option to treat your knee wrist arthritis.The exact type of work depends on age, anatomy and major condition.Some examples of surgical options to treat arthritis include osteotomy consisting of a cutting bone to align the wrist and the knee replacement operation.
Modern methods of treatment Arthrosis knee wrist include osteotomy, which is a good alternative if patient young and arthritis is limited by one area of the knee joint.This allows the surgeon to restore the knee to unload the area of arthritis and executed the load relatively not included parts of the knee wrist.For example, the patient can be renewed for redistribution of loads through the joint.The advantage of this type of operation is that the patient's common knees are preserved and can potentially provide multi-annual pain benefits without disadvantages of prosthetic knees.Disadvantages include a longer rehabilitation course and the possibility of arthritis development in recently straightened knee.
The operation operation of the knee joint involves cutting the arthritic bone and insert a prosthetic compound.All arthritic surfaces are replaced, including a femur, reluctant leg and knee cup.Arthritic surfaces are removed, and the ends of the bones replace the prosthesis.The prosthetic component is usually made of metal and plastic surfaces, which are designed for smooth slipping towards each other.
Knee joint replacement
The overall operation for replacing the knee joint was performed for the first time in 1968. and over the years of developing in a reliable and efficient way to resolve pain when it turns off and enables patients to continue with active life.Implements in the field of surgical methods and implants have helped this from the most successful orthopedic procedures today.As the population becomes older and remains more active, the need for general knee replacement continues to grow.Many knee joint replacements were held in the hospital of special operations.Improvements to surgical technology and new implant design are some of the contributions that have been performed by surgeons.
People often wonder when and why should you replace the knee.This is an individual issue that depends on the level of human activity and functional needs.Many people with arthrosis live with pain, which prevents them from participating in activities;Others are so weakened to be hard for their shoes and socks.The complete replacement of the knee joint offers a solution to the problem of arthrosis and is done to mitigate the activity of pain and continuation.After rehabs from a successful complete replacement of the common knee, the patient can expect surgery, without pain.Complete replacement of the knee joint significantly improves the patient's condition and significantly reduces its long-term treatment costs.This study has shown that not only the total reinforcement of the knee joint does not exist economically effective in relation to non-jarse control, but also provides greater functionality and the best quality of life.
The complete replacement of the knee joint is considered great operation, and the solution is not trivial.Usually people decide to undergo surgery when they feel that I can't live with my arthritis anymore.The implant consists of 4 parts: tibia, thigh parts, plastic inserts and patients.Components of tibia and femur are made of metal, usually cobalt chrome, used to close the ends of thighs and lower legs after removing the arthritis bone.The plastic artist is made of polyethylene ultra -high molecular mass and fits into a tibi component, so the polished thigh belt slides with plastic.The knee chicken component also slips the front of the femoral component.They are usually attached to bone cement.
Full knee replacement is performed in an operating room with a special air flow system laminar, which helps reduce the likelihood of infection.Your surgeon will carry "SpaceSuit", also designed to reduce the likelihood of infection.The entire surgical team will consist of your surgeon, from two to three assistants and nannies.
Anesthesia is given through an epidural catheter that is a small pipe inserted in the back.It is the same type of anesthesia given by women in childbirth.During surgery, the patient can be both awake and sleepy.
After the introduction of an epidural block around the thigh, the tournament or cuff will be placed.The horizontal bar will be overestimated during the work for reducing blood loss.The neckline for complete change of knees is made with the front knee.The cut will measure 4 to 10 inches depending on the anatomy.
Arthritis of the femur, lower legs and patients were exposed and removed using strength tools.At the same time, the knee deformations were corrected, and after surgery, the knee becomes straight.The bone is ready to take the artificial joint of the knee, and then a prosthesis is inserted.During closure, two drainage are installed around the work area to help evacuate blood.The papers are used to close the skin.
The entire operation will last from 1 to 2 hours.After that, the patient will be taken to the recovery room in which tests will be checked.Most patients can be taken to a regular room for several hours;Others will have to stay in the recovery hall, as defined by a surgeon and anesthesiologist.

Patients usually remain in hospital 3-4 days after the full knee replacement operation.
Risks during surgery
Some of the risk of surgery include blood loss, the formation of clot in the leg and the likelihood of infection.The general prevalence of these risks is very small.They should talk about the surgeon before the operation begins.
Some of the risks of the presence of prosthetic knees include the likelihood that parts can weaken or wear over time, or the prosthesis can be infected.Again, these issues will be discussed with the surgeon.
Postoperative course
Immediately after full work for replacing the knee joint, the patient will fall into recovery room.Most patients can enter the regular department after a few hours, when the sensation returns to your feet.The hospital pump is given to the epidural category associated, which will allow you to control when it is given a cure for pain.Most people are quite pleasant with the help of pulp pumps.
On the day of work you can perform some exercises, as indicated by the physiotherapist, including the reduction of quadriceps and moving legs up and down.Depending on the surgeon preferences, you can start bending your new knee immediately after surgery or on the first day.The patient will be allowed to attend LED after surgery to moisten his mouth, but drink liquids or you can cause nausea.The patient will have a catheter in the bladder, so you don't have to worry about urinating.As soon as they start in the legs of recovery, it will be allowed to sit, get up and take a few steps with a walker and a therapist.
The first day after surgery will be active, developed to help the cell phone station.The Pacrant will meet with physiotherapists to refer additional exercises.In addition, it will help enter their feet and take a few steps with a walk.As a rule, the patient will be allowed to drink a clean liquid.
In the next few days it will be easier and easier to move.The patient will be released from the pain and urinary catheter.Pain treatment will be given in the form of a tablet.On the second day after surgery, if the signs of recovery are in the guts, they will be allowed to eat ordinary food.
Depending on your age, preoperative physical condition and coating insurance, the patient can be a candidate for short accommodation in the rehabilitation facility.Otherwise the patient will be dropped home, and the physiotherapist will come to his house to continue rehabilitation.The dispatcher will discuss these options with the patient and will help him plan back home.
The return of activities will lead the surgeon and therapists.As a rule, patients can walk as much as they want 6 weeks after surgery.Patients can continue movement after 6 weeks.After 8 weeks, patients can continue playing in golf and swimming;In 12 weeks I can play tennis.The surgeon will help decide which actions can continue.
That requires a physiotherapist
All physical therapists prepare through education and clinical experience to treat various conditions or injuries:
- Physiotherapist having experience in treating people with osteoarthritis of the knee wrist and after the knee joint replacement surgery.Some physiotherapists have practices with an orthopedic focus.
- Physiotherapist, which is a certified orthopedic clinical specialist.This physiotherapist will have advanced knowledge, experience and skills that can be applied to the state.
- You can find physiotherapists that have these and other accounting data using MRI, network tool to help find physiotherapists with specific clinical knowledge.
General advice When you can find a physiotherapist (or any other medical service provider):
- Get family and friends recommendations or from other suppliers of medical services;
- Converting to a physiotherapy for reception, you need to ask about the experience of physiotherapists in providing help people with arthritis.
During the first visit with a physiotherapist, you must be willing to describe the symptoms as much as possible and report on activities that worsen the symptoms.
































